Hepatocellular Carcinoma
Overview
- HCC is the sixth most common cancer, the third leading cause of cancer-related deaths, and the second most lethal cancer. It represents 90% of primary liver cancers and occurs in the presence of underlying cirrhosis most of the time
- Patients with chronic HBV infection and patients with NAFLD/MAFLD can develop HCC in the absence of cirrhosis
- Patients with cirrhosis (Child Pugh A or B or those patients with Child Pugh C awaiting liver transplantation) and patients without cirrhosis with chronic HBV infection at increased risk of HCC should undergo HCC surveillance with ultrasound and AFP every six months
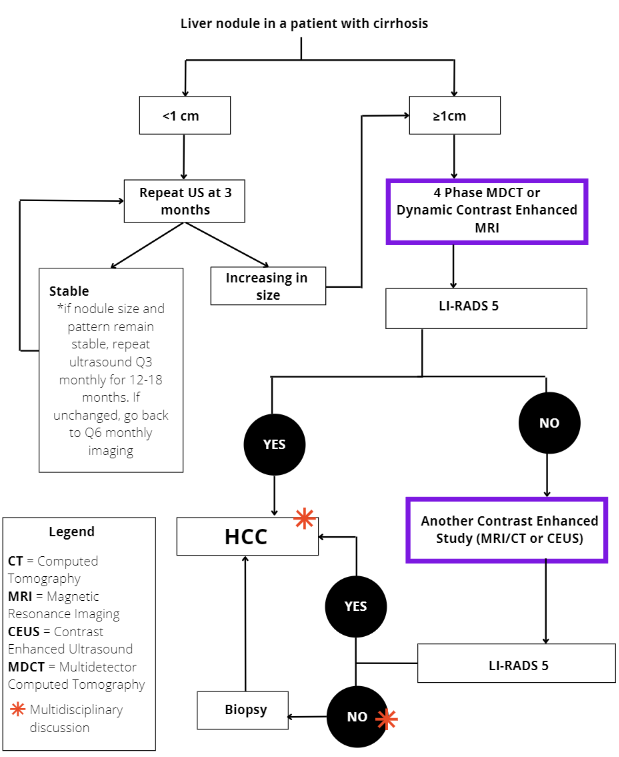
- The diagnosis of HCC in patients with cirrhosis is based on dynamic imaging (e.g. CT, MRI or CEUS) according to well-defined criteria. Liver biopsy is needed to confirm the diagnosis in cases with atypical imaging features and in all patients without underlying cirrhosis
- Staging and treatment allocation are based on the Barcelona Clinic Liver Cancer (BCLC) staging system, which takes into account the tumor burden, the underlying liver function, and the patient’s performance status
- All patients with HCC must be reviewed at a Multi-Disciplinary Team (MDT) meeting before selecting therapy. This approach has increased survival rates in other series. Within Alberta, this occurs in Edmonton and Calgary
Risk Factors and prevention
- The most important risk factor for HCC is liver cirrhosis. Hence, to prevent progression to cirrhosis, it is very important to detect chronic liver diseases in the general population early on in their natural history. Other risk factors for HCC are age, male sex, diabetes, obesity, alcohol, tobacco, and aflatoxin B1 exposure
- Primary prevention should aim to prevent chronic liver disease by promoting a healthy diet, exercise, responsible drinking, and HBV vaccination
- Secondary prevention should target the treatment of the etiology of the underlying liver disease, and other risk factors associated with HCC, in order to prevent disease progression and development of HCC. Coffee drinking may protect against HCC
Note: Tertiary prevention would aim to reduce the risk of recurrence after curative treatments, but so far, there are no neoadjuvant or adjuvant therapies approved for this purpose.
Who should be screened:
- Patients with cirrhosis (regardless of the etiology) who are Child Pugh A or B
- Given limited treatment options, surveillance should only be done in Child Pugh C patients if they are eligible for liver transplantation
How to screen:
- Ultrasound surveillance with serum alpha-fetoprotein (AFP) every six months. Overall sensitivity of the ultrasound is 84%, but only 45% for early stages; the addition of AFP increases sensitivity to 63% in early stages
- Do not use AFP alone for surveillance
NOTE: Ultrasound may perform sub-optimally in patients with obesity, steatosis, and/or multinodular livers. The US LI-RADS visualization score (i.e. A for minimal limitations, B for moderate limitations, and C for severe limitations) can help identify the need for an alternative screening strategy in a given patient (e.g. cross-sectional imaging).
All patients with HCC must be reviewed at a Multi-Disciplinary Team (MDT) meeting before selecting therapy.