Ascites
Overview
- For people with cirrhosis and new onset or known ascites worrying signs or symptoms are abdominal pain, fever, worsening kidney function, and confusion
- Perform a diagnostic paracentesis along with a history, physical and labs in any patient presenting to the emergency room, or those with symptoms or signs of infection, kidney dysfunction or encephalopathy
- Patients with ascites may be candidates for a transjugular intrahepatic portosystemic shunt (TIPS) or for liver transplantation
- Non-selective beta blockers (NSBB’s) and other blood pressure lowering medications may need to be adjusted in patients with ascites
- If a patient has decompensated cirrhosis consider contacting a liver specialist to discuss management advice and potential transplant candidacy
Blood work:
- Basic labs (CBC, electrolytes, creatinine, albumin, PT, bilirubin, ALT)
- Blood cultures (if suspicion for spontaneous bacterial peritonitis, polymorphonuclear cell count >250 cell/ml)
Ascites fluid analysis:
- Fluid cell count and differential
- Fluid culture and sensitivity (inoculate fluid directly into blood culture bottles)
- Fluid prorenin
- Fluid albumin
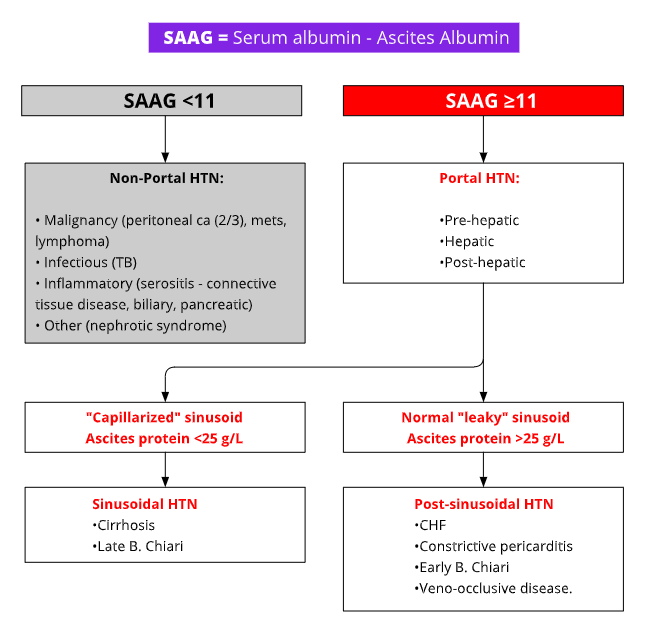
- Ascites in cirrhosis (SAAG >11 g/dL, protein <25 g/L)
- If certain diagnoses are suspected, additional testing may be needed: fluid cytology (malignancy), lipase (pancreatitis), triglycerides (chylous ascites), bilirubin (bile leak), TB culture (tuberculosis)
General Principles
- Tips for advising sodium restriction ≤ 2 grams/day: be aware that this reduces diet palatability and intake. Consult a dietitian and provide resources such as Cirrhosis Care Alberta, Cirrhosis Care - Cirrhosis Nutrition, and The Nutrition in Cirrhosis Guide
- Hold medications that predispose to fluid retention/kidney dysfunction, e.g. NSAIDS, amino glycosides, angiotensin-converting-enzyme inhibitors, angiotensin II antagonists or alpha1-adrenergic receptor blockers
- Start diuretics and/or consider TIPS
- There is no need for fluid restriction unless hyponatremia is severe or sudden
- Promote patient self-management for ascites
- Consider contacting a liver specialist to discuss management advice
- Alcohol intake should be stopped
General Principles
- The mainstay of therapy for ascites is sodium restriction + diuretics. Spironolactone and furosemide are often given in combination in a ratio of 50 mg (spironolactone) to 20 mg (furosemide). In cases of mild ascites, spironolactone monotherapy may be enough
- Large volume paracentesis (≥ 5 L drained) is required for tense or refractory ascites. Give IV albumin (100 cc of 25% albumin (25 grams) for every 3 L ascites removed). With kidney dysfunction or hypotension, be more cautious with the amount of fluid that is drained off
Spironolactone Monotherapy
- 50-100 mg orally in the morning
Amiloride (Substitute for Spironolactone)
- Starting dose of 10 mg, where 10 mg = 100 mg of Spironolactone
- Maximum does: 40 mg
Dosing for Combination Diuretics
- Starting dose: Spironolactone 50-100 mg in combination with Furosemide 20-40 mg orally in the morning
- If the electrolytes and creatinine remain normal, doses can be increased in increments of 50-100 mg Spironolactone to 20-40 mg Furosemide after 4-7 days
If hyperkalemia develops, reduce Spironolactone
- The Spironolactone to Furosemide ratio of 50 mg:20 mgoften works to balance electrolytes, but must be individualized
Large-volume (≥ 5L) paracentesis AND start combination diuretics if no contraindications
- Give 25% Albumin 100 cc for every 3 liters removed
If concern about spontaneous bacterial peritonitis or patient has kidney dysfunction, do not remove >5 liters over 24 hours
- Remove paracentesis catheter the same day
- Diuretic-induced complications (renal dysfunction, hyponatremia)
OR
- Non-response to diuretics
- Continue regular large volume paracenteses alongside general management. At each elective paracentesis do a Fluid cell count and differential and Fluid culture and sensitivity
- Encourage compliance with sodium restriction, alcohol abstinence, monitor electrolytes, creatinine
- The dose of non-selective beta-blockers may need to adjusted in some patients with refractory ascites
- Non-selective beta-blocker (NSBB) use in Refractory ascites
- In patients with Refractory ascites and (i) systolic blood pressure <90 mm Hg, or SCr >133 umol/L or (iii) sodium <130 mmol/L reduce or temporarily discontinue NSBBs
- If paracentesis ≥ once a month:
- Discuss alternative therapies with a Liver specialist if this hasn’t been done already (i.e. TIPS, transplantation, indwelling peritoneal catheter)
- Q weekly weights (daily weights whole diuretic dose is being titrated): aim for up to 0.5 kg of fluid loss per day
- Q 1-2 weekly creatinine and electrolytes as doses are being increased. Extend to Q 2-3 monthly once tolerating a stable dose
- Reduce/Stop if: Na+ ≤ 125mmol/L or worsening kidney function, or symptomatic hypotension
- Increase every 4-7 days as tolerated
- Can double doses if weight loss <2 kg a week and creatinine, electrolytes are stable.
- Adjust more cautiously once peripheral edema has cleared
- Maximum doses are Furosemide 160 mg, Spironolactone 400 mg (see Spironolactone/Furosemide dosing ratio)
- If there is an inadequate response to diuretics, you can use the urinary sodium to check for dietary non-compliance or resistance to diuretics.
- The 24 hour urine or spot urine electrolytes can be used to evaluate
- #1: Dietary non-compliance – If the Spot urine Na/K ratio is >1 OR the 24-hour urinary Na excretion is 78 mEq/day in a patient on diuretics who is not losing weight. This means the patient is sensitive to diuretics but not adherent to sodium restriction.
- #2: Diuretic resistance – If the Spot urine Na/K ratio is 1 OR 24-hour urinary Na excretions is <78 mEq per day in a patient on maximally tolerated diuretics who is not losing weight. This mean the patient is resistant to diuretics